For decades, the scientific community has grappled with the enigmatic nature of neuropathic pain—a debilitating condition that arises from damage or dysfunction in the nervous system. Unlike acute pain, which serves as a vital warning signal, neuropathic pain often persists long after the initial injury has healed, becoming a disease in its own right. Recent breakthroughs in neuroscience have unveiled a revolutionary approach to understanding this complex phenomenon: decoding the "spinal cord cipher" that underlies pain perception. Researchers are now mapping the specific neural circuits responsible for neuropathic pain, offering hope for targeted therapies that could alleviate suffering for millions.
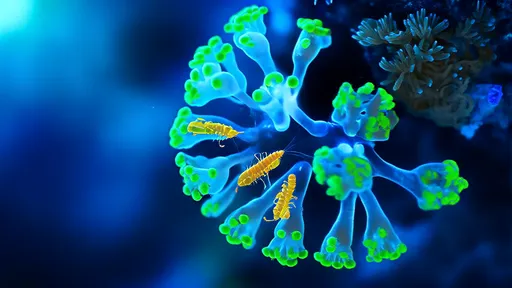
The concept of a "spinal cord cipher" refers to the intricate pattern of neural activity that encodes pain signals as they travel from peripheral nerves to the brain. This cryptographic analogy highlights the complexity of pain processing, where subtle variations in signaling can mean the difference between protective sensation and chronic agony. By deciphering this code, scientists aim to identify the precise pathways that become aberrant in neuropathic pain states. Early studies using advanced optogenetics and single-cell sequencing techniques have revealed startling specificity in how these circuits malfunction, challenging long-held assumptions about pain as a monolithic experience.
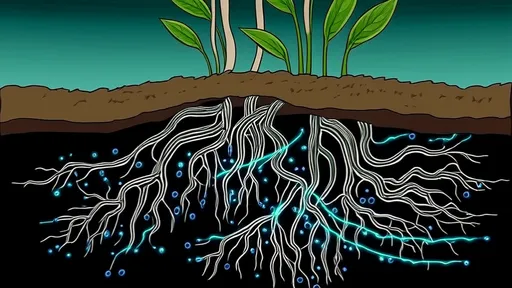
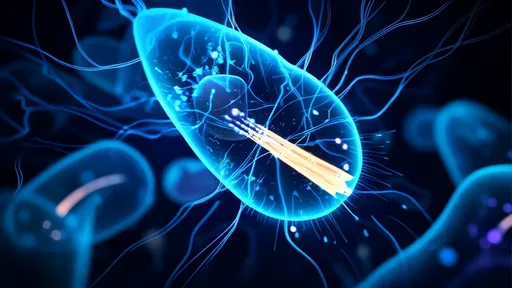
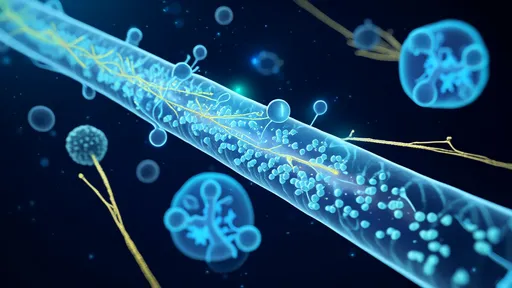
At the forefront of this research are teams employing cutting-edge viral tracing methods to visualize pain pathways with unprecedented resolution. These approaches allow scientists to follow individual neurons from their peripheral origins through spinal cord relays to higher brain centers. What emerges is not a simple linear pathway but an elaborate network with multiple decision points where pain signals can be amplified, dampened, or distorted. Particularly intriguing are the discoveries about microcircuits within the dorsal horn of the spinal cord—a critical gateway where sensory information is first processed before ascending to the brain.
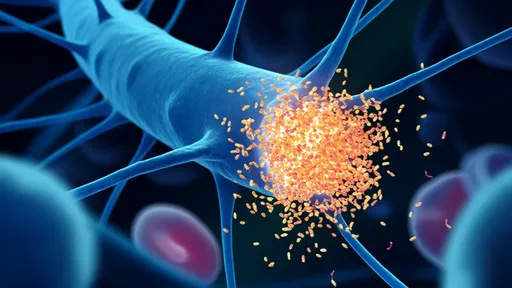
The implications of these findings extend far beyond academic curiosity. Current treatments for neuropathic pain, including opioids and anticonvulsants, often prove inadequate or come with severe side effects because they target broad neural mechanisms. The new circuit-based understanding suggests that precision interventions could be developed to correct specific malfunctions in the pain cipher without disrupting normal sensory function. Several research groups are already testing this approach in animal models, using genetically targeted therapies to silence hyperactive pain circuits while sparing surrounding neural activity.
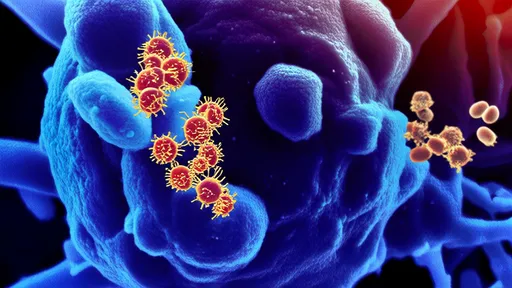
One particularly promising avenue involves identifying molecular markers that distinguish pathological pain circuits from normal ones. Recent work has uncovered distinct populations of spinal neurons that become "hijacked" during neuropathic pain development, essentially creating a new cipher that perpetuates pain signals even in the absence of ongoing tissue damage. These neurons exhibit unique genetic signatures and connectivity patterns that make them ideal targets for next-generation analgesics. Some experimental compounds that home in on these molecular markers have shown remarkable efficacy in preclinical trials, reducing neuropathic pain symptoms without the sedating effects of current medications.
The clinical potential of this research cannot be overstated. Chronic neuropathic pain affects approximately 7-10% of the population worldwide, with conditions ranging from diabetic neuropathy to postherpetic neuralgia and phantom limb pain. Many patients cycle through multiple ineffective treatments before finding partial relief, if any. The ability to classify neuropathic pain subtypes based on their underlying circuit abnormalities could revolutionize diagnosis and treatment selection. Imagine a future where a simple diagnostic test could reveal which specific cipher has gone awry in a patient's nervous system, guiding physicians to prescribe therapies tailored to correct that exact dysfunction.
As the field progresses, researchers are confronting both technical and conceptual challenges. The spinal cord's dense architecture makes it difficult to observe circuit activity in real-time, especially in awake, behaving animals. Moreover, the relationship between neural activity patterns and subjective pain experience remains partially understood. New imaging technologies and computational models are helping bridge these gaps, allowing scientists to correlate specific circuit dynamics with pain behaviors more accurately. International collaborations are forming to create comprehensive atlases of pain circuits across different neuropathic conditions, much like the Human Connectome Project mapped healthy brain connectivity.
Ethical considerations accompany these scientific advances. The prospect of precisely manipulating pain circuits raises questions about enhancement versus therapy—where to draw the line between alleviating suffering and augmenting normal function. Additionally, the translation of these discoveries into clinical applications must proceed carefully to avoid unintended consequences of circuit modulation. Researchers emphasize the need for rigorous safety testing as these targeted approaches move toward human trials, likely within the next five to ten years for the most advanced candidates.
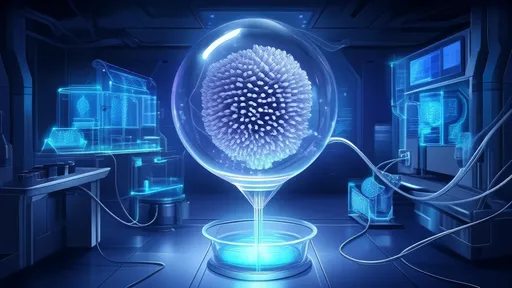
Beyond pharmaceutical interventions, the circuit-based understanding of neuropathic pain is inspiring novel neuromodulation devices. Traditional spinal cord stimulators work through crude electrical pulses that affect broad neural populations. Next-generation implants in development aim to interact with the nervous system's natural cipher, detecting pathological activity patterns and delivering precisely timed interventions to normalize circuit function. These "closed-loop" systems could provide real-time correction of aberrant pain signaling while minimizing side effects. Early prototypes have shown promise in animal studies, adapting their stimulation parameters dynamically as pain circuits fluctuate.
The decoding of pain's spinal cipher represents a paradigm shift in how we understand and treat neuropathic conditions. No longer viewed as merely a symptom to suppress, chronic pain is increasingly recognized as a disorder of specific neural circuits that can potentially be repaired or reprogrammed. This research trajectory offers hope that we may one day transform neuropathic pain from a life sentence to a treatable condition, restoring quality of life for countless individuals. As mapping efforts continue to refine our understanding of pain's neural alphabet, the possibility of truly personalized pain medicine draws closer to reality.

By /Aug 18, 2025
By /Aug 27, 2025

By /Aug 27, 2025
By /Aug 18, 2025
By /Aug 27, 2025
By /Aug 27, 2025
By /Aug 18, 2025
By /Aug 18, 2025
By /Aug 18, 2025

By /Aug 18, 2025

By /Aug 18, 2025
By /Aug 18, 2025
By /Aug 27, 2025
By /Aug 18, 2025
By /Aug 18, 2025

By /Aug 18, 2025

By /Aug 18, 2025
By /Aug 18, 2025

By /Aug 18, 2025
By /Aug 18, 2025